Action from learning report 2023/24
Addressing health inequalities and preventing premature and avoidable deaths among people with a learning disability and autistic people

Summary
This report is for health and care staff, integrated care system (ICS) strategy leads and commissioners across England. It shares insights and resources from quality improvement initiatives that address the health inequalities people with a learning disability and autistic people experience. It supports NHS England’s commitment to improve health outcomes for people with a learning disability and autistic people and the 2025/2026 NHS priorities and operational planning guidance, which requires integrated care systems (ICSs) and NHS trusts to work together to reduce inequalities. This report will likely also be of interest to people with a learning disability, autistic people and their families and carers. An easy read version [add hyperlink] is also available.
Overview
The recent LeDeR annual report highlights the significant health inequalities people with a learning disability and autistic people still face. This Action from Learning report showcases examples of work that continues to be done locally to address LeDeR findings.
Each of the 8 featured case studies demonstrates how, through focused improvement work, local systems are implementing robust approaches to:
-
safeguard people with a learning disability and autistic people from avoidable harm and prevent poor experiences of care
-
meet their statutory duties around reducing inequalities
-
uphold patient safety standards
They share learning about practical implementation, impact and outcomes and provide resources to support adoption and spread of the initiatives across England.

Call to action
We encourage system leaders and health and care professionals to take action and implement similar quality improvement work locally, with the approaches tailored to local contexts and population needs.
The analysis of findings from local LeDeR reviews should inform which areas organisations within each ICS should prioritise for this quality improvement activity.
NHS trusts should ensure their staff know to notify the deaths of people with a learning disability and autistic people to LeDeR. This will continue to build robust local evidence for the aspects of care that need to be better and, importantly, afford bereaved families access to LeDeR reviews.
Related resources
People stories

Jodie Williams, Learning Disability and Autism Network Manager, NHS England
I work at NHS England as a learning disability and autism network manager. I have a mild learning disability and type 1 diabetes. I live with my assistance dog Mindy who goes everywhere with me. I think it is really important that the NHS helps people like me who have diabetes or other long-term conditions to get better healthcare.
When I have appointments with health services I need some reasonable adjustments. For me this means using easy read information, sometimes having my mum at appointments with me but the one that helps most is having my assistance dog Mindy with me. Mindy helps keep me calm especially when I have blood tests or injections, and I like the sensory feeling of stroking her if I am worried.
In this Action from Learning report we are sharing stories of good things that have happened in different areas in England to help people with a learning disability and autistic people have longer and better quality lives. We need people to carry on notifying deaths to LeDeR so the NHS can carry on learning, improving and making things better for people like me.

Carl Shaw, Learning Disability and Autism Adviser, NHS England
I work on LeDeR in the Health Improvement Team at NHS England and I am someone with a mild learning disability. I have 2 children in my life who I care for. They are both diagnosed with autism and ADHD. It is very important to me that they live a long, happy and healthy life. I learn important things from LeDeR like making sure to take care of my eyesight, dental health, incorporating exercise and that eating a healthy diet can help me live longer. These are important things to teach the children I care for.
It is important to me that professionals and services also learn through LeDeR to help people live long lives like everyone else. Taking on board the views of families and carers, including those who have taken part in LeDeR reviews, will help us to change services in a way that will make a difference.
Someone with a learning disability from an ethnic minority community could die even younger than someone who is white. This is not OK and we need more people to notify and review the lives and deaths of people from ethnic minority communities so health services can learn and take action.
The deaths of autistic people have been notified to LeDeR from 2022 but we know we are not getting all the deaths notified so the information is not very reliable. We need everyone to report the deaths of autistic people to LeDeR because the numbers are still low. Every time a life and death is reviewed there is more learning, which means we can improve services for people like me.
Improvement work across the country
The following examples describe actions that system partners and their health and care staff have taken to improve access, people’s experience of using services and their outcomes. Local LeDeR annual reports on ICB websites list and give more detail of local service improvement work.
Making a primary care network autism friendly – London
Autistic people can experience significant health inequalities and reduced life expectancy compared to the general population (UK Parliament, 2024). The NHS Long Term Plan set out the steps the NHS should take to tackle the causes of ill health and preventable death for autistic people and to improve their experience of using health services.
The challenge
London Fields Primary Care Network (PCN) comprises 6 GP practices in the City of London and Hackney. The PCN wanted to improve access to primary care services for autistic people by making its practices more autism friendly and giving them more support from practice staff.
The response
 Between May 2022 and March 2024 the PCN implemented a scheme to make its services more accessible and ‘autism friendly’, by ensuring its staff have the training and learning opportunities around autism they need to build confidence in implementing reasonable adjustments for autistic people.
Between May 2022 and March 2024 the PCN implemented a scheme to make its services more accessible and ‘autism friendly’, by ensuring its staff have the training and learning opportunities around autism they need to build confidence in implementing reasonable adjustments for autistic people.
The project lead ran 2 surveys – 1 for staff and 1 for autistic adults and those who support them, as well as interviews with the latter group.
Staff identified that, to feel more confident to work with autistic people and implement reasonable adjustments they needed:
- clear guidance on how to best support autistic people
- autism training, including on how to recognise autistic traits or that a person has more than one condition: for example, dyspraxia or ADHD as well as autism
- opportunities to listen to people’s lived experiences of autism
68% of autistic people and those who support them said it was difficult to go to their GP; 44% reported that the practice environment was ‘hard’ or ‘very hard’ to manage; and 32% did not know what to expect during their appointment. Respondents suggested areas for improvement:
- staff being aware of the person’s needs or reasonable adjustments or asking them how their visit could be made more comfortable
- staff understanding autism; responders said knowledgeable staff help reassure and make them feel less anxious staff having the time to explain things clearly in the way that works best for the person and giving them time to process information
- contact in ways other than phone calls as some people find these provoke anxiety
- making the physical environment of the GP practice or healthcare setting more welcoming to autistic people: for example, having a quiet space or sensory tools like ear defenders or picture books available
The outcome
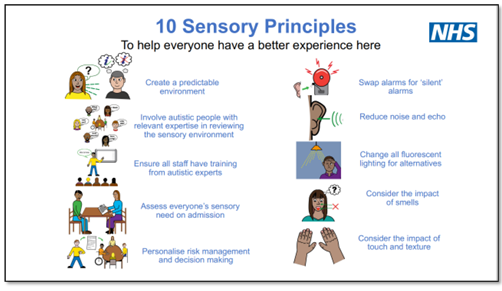
Based on the above insight, the project steering group, which included experts with lived experience, developed materials to make health and care practices and the wider neighbourhoods more autism friendly:
- City and Hackney autism friendly standards. These help healthcare providers, public sector and community organisations understand what it means for their services to be autism friendly and more accessible to autistic people. The standards set goals such as celebrating autism acceptance, making things predictable and creating a sensory friendly environment.
- Autism friendly checklists for primary care and other healthcare settings (now embedded in GP commissioning contracts) – tools for the PCN and healthcare staff to self-assess the accessibility of their service for autistic people and then create a plan to make any improvements and reasonable adjustments, including providing people with alternative methods of contact for appointments, longer appointments, advice on what to expect or a quiet space to wait.
- A learning pack for reception staff on supporting autistic people; 300 have already accessed this. A top tips guide for supporting autistic adults during appointments is also available. Some GP practice staff also attend autism training that is co-designed and co-delivered with an autistic resident.
 GP practices that complete the checklist and their plan to improve accessibility where staff have accessed the training, receive a City and Hackney autism friendly badge.
GP practices that complete the checklist and their plan to improve accessibility where staff have accessed the training, receive a City and Hackney autism friendly badge.
Wider impact
Homerton Hospital A&E department, among other facilities, is implementing actions to make it more accessible for autistic people and people with a learning disability, with help from the Homerton Learning Disability and Autism team. These include:
- asking the people if they need reasonable adjustments when they book in
- providing guidance to staff on what they should do when an autistic person presents at A&E
- providing sessions for staff on how to support people with a learning disability and autistic people
- providing a quiet space for people to wait where possible
Contact
For more information, please contact
Resources
-
NHS England: Sensory friendly resource pack. This supports the delivery of the NHS Long Term Plan commitments for autistic people and adjustments to the sensory environment of NHS settings.
-
City and Hackney: Autism friendly checklists for primary care and health care settings
-
LeDeR resource bank – reasonable adjustments
- NHS England: The Oliver McGowan mandatory training on learning disability and autism
Reviewing the quality of annual health checks – Coventry and Warwickshire
 The NHS Long Term Plan set the ambition that by 2023/24 at least 75% of people aged 14 and over on the learning disability register in England should receive an annual health check (AHC). Due to the work of NHS primary care staff, community learning disability teams, self-advocates, families, carers and others this national target rate was surpassed early – 79.8% in 2022/23.
The NHS Long Term Plan set the ambition that by 2023/24 at least 75% of people aged 14 and over on the learning disability register in England should receive an annual health check (AHC). Due to the work of NHS primary care staff, community learning disability teams, self-advocates, families, carers and others this national target rate was surpassed early – 79.8% in 2022/23.
When done properly AHCs promote healthy lifestyles, support wellbeing and enable early access to healthcare support if the person needs this. They can spot early signs of cancer, diabetes, respiratory and heart disease, and provide an opportunity to discuss vaccinations, promote screening, manage and monitor known health conditions such as epilepsy or dysphagia (swallowing difficulties) and discuss end of life decisions.
For an AHC to qualify as a good one, practices need to create a health action plan with the person, outlining the person’s health needs, what they need to stay healthy and who can help them with this, and a next review date.
The challenge
In 2022/23, NHS Coventry and Warwickshire ICB achieved an AHC uptake of 81% and for 96% of these a health action plan was completed. Despite this substantial improvement, regional learning from LeDeR showed inconsistencies in AHC quality and the level of detail recorded in health action plans. Also, 848 eligible people did not receive an AHC in 2022/23 (based on learning disability register data as of March 2023).
The response
In 2023/24 the ICS’s Quality and Nursing Clinical Transformation Team evaluated the quality of AHCs and health action plans and sought to understand why some people have never received an AHC or not in the last 3 years.
Evaluating the quality of AHCs. The team developed an AHC service evaluation form and invited GP practices across Coventry and Warwickshire to complete this; 8 took part. The form asked:
- Were patients sent an accessible invitation?
- Did they receive a pre-AHC questionnaire? (these can reduce a person’s anxiety and help them or their carers think about what they want to ask the GP or nurse at their AHC)
- Were they offered reasonable adjustments and their needs flagged?
- Was their ethnicity and level of learning disability (mild, moderate, severe) recorded? (recording of both is mandatory)
- Did they receive a health action plan documenting what is needed to help them stay healthy?
Learning disability nurses reviewed 32 AHCs from GP notes – for 1 man and 1 woman aged 65 or over, a young person between 14 and 17 years and a younger woman over 25 years at each of the 8 practices. (LeDeR learning had established particular health inequalities in the area for transition from young people’s services, and for bowel, breast and cervical screening.) They found:
- ethnicity inconsistently recorded and level of learning disability not recorded in 12%; staff training was recommended as well as further review to identify any correlation between this level and quality of AHC received
- only 60% received a pre-AHC questionnaire
- reasonable adjustment digital flags were not added to every person’s medical record
- no conversation about transition to adult services had been with over half the young people
- low uptake of relevant cancer screening compared to the general population: bowel cancer (54%), breast cancer (18%), cervical cancer (33%). Some good practice was identified – a person had bowel screening at their AHC and another had a breast examination. The ICS is working to address screening uptake
- low uptake up of the pneumococcal vaccination. A local LeDeR sub-group is working to addressing this. Some good practice was identified – a person at risk of respiratory illness received pneumococcal vaccination at their AHC
- for the 32 people whose AHC was reviewed, only 16 had a health action plan. Some good practice was identified: well-documented plans with action points including an ECG for 1 person and referral to physiotherapy for another with Parkinson’s disease; 1 person’s medication was reviewed and their anti-psychotic medication reduced
The nurses also spoke to 22 people who received an AHC or their carer/family member about their experience and found:
- reasonable adjustments, home visits and adapted communication are valued
- some felt rushed and wanted more time to discuss their health
- 3 carers said an AHC would not have happened without a home visit
- 1 patient could not remember receiving their AHC (it was done in a telephone call)
Evaluating why some people had not received an AHC. The team asked 20 people or their family/carer (5 from each of 4 GP practices with 10 or more eligible people who did not receive an AHC in 2022/23) why they had never had an AHC (over half) or not in the previous 3 years. Their reasons included:
- see a paediatrician and do not feel an AHC is needed (2 people)
- health needs already met by GP (4)
- cannot recall receiving an invitation for an AHC (5)
- already have other health checks: for example, for mental health
- lack of support to travel to the appointment or no reasonable adjustments to support attendance – for example, struggle with the practice environment, receiving a text invitation but do not read texts
and they suggested that the following would help them have an AHC:
- combine with other GP appointments
- having an AHC at home (8 of 20)
- send an easy read invitation rather than a text
- provide support to attend an AHC (3 in 20)
 Learning disability friendly badge: In September 2023 the ICB launched a scheme it had developed with the charity Grapevine and a group of GPs to maintain the high AHC uptake in the area and ensure their GP practices met a quality standard. Those GP practices meeting the scheme’s good practice criteria – provides reasonable adjustments, personalised care and high quality AHCs and has an identified learning disability champion – can apply for a ‘learning disability friendly’ badge and be accredited as a ‘learning disability friendly’ practice.
Learning disability friendly badge: In September 2023 the ICB launched a scheme it had developed with the charity Grapevine and a group of GPs to maintain the high AHC uptake in the area and ensure their GP practices met a quality standard. Those GP practices meeting the scheme’s good practice criteria – provides reasonable adjustments, personalised care and high quality AHCs and has an identified learning disability champion – can apply for a ‘learning disability friendly’ badge and be accredited as a ‘learning disability friendly’ practice.
The outcome
In 2023/24, GP practices in Coventry and Warwickshire delivered more AHCs than in 2022/23, despite the ICB not commissioning targeted AHC support for learning disability nurses.
So far 13 GP practices have been accredited as ‘learning disability friendly’ and the application panel will review more when they next meet. This panel includes a LeDeR reviewer and representatives from Grapevine, the ICB’s primary care and/or quality team, and the Community Learning Disability Team.
Wider impact
In summer 2024 the ICB published its findings and recommendations for best practice, sharing these across the ICB, primary care and nationally.
Contact
For more information please contact:Resources
- Coventry and Warwickshire ICB: Annual Health Checks Quality Report
- Coventry and Warwickshire Learning Disability Friendly Badge – application form for GPs
- Coventry and Warwickshire: Guidance for health and care staff on annual health checks
- LeDeR resource bank
The 2023 LeDeR Annual Report found that respiratory diseases are the second most common cause of death among people with a learning disability, accounting for 16.5% of deaths in 2023 compared with 11.1% in the general population in 2022.
A rapid response respiratory service – Lincolnshire
The challenge
The children’s physiotherapist at Lincolnshire Community Health Services NHS Trust was profoundly affected by the death in 2018 of a child with complex needs they had treated during repeated admissions to hospital with chest infections.
The physiotherapist reflected that preventing, diagnosing and managing poor respiratory health at home would be a better way to care for the children they see in hospital, many of whom have cerebral palsy and over 80% a learning disability.
Clinicians observed that the young people under their care who were not mobile or who needed support for movement experienced recurrent chest infections or long-term ventilation.
The response
In 2019 the physiotherapist and a colleague established a pilot scheme of support for parents and carers of children with complex respiratory needs to do some physiotherapy, as well as a visit when any child or young person at home became ill for example, at the start of a cough – to deliver treatment. Without this visit the child or young person would likely have seen a GP or attended hospital, and potentially been admitted.
Based on the success of the pilot in reducing hospital admissions and with recurrent funding for an expanded physiotherapy team, in February 2020 the team established the 5-day Lincolnshire Complex Needs Rapid Response Respiratory Service – a new pathway to avoid hospital admissions/readmissions for children and young people aged 19 and under with complex respiratory needs. Since 2023, this has been an all age, 7-day service.
A physiotherapist visits the person within 48 hours of being notified by a parent or carer that they are unwell, but in practice this is usually on the same day. People are seen at home, in school, in care homes and even at holiday sites. The physiotherapists provide treatments to keep the person well: for example, airway suction, chest percussion and use of cough assist machines. Some can prescribe antibiotics and others are training to qualify as prescribers. The physiotherapists also assess the child’s chest using a risk identification matrix to identify the risk of recurrent chest infections.
Where the person needs further support, the team can contact the local district general hospital, nearby tertiary centres and other community services to request advice from consultants, nurses or palliative care teams.
If a person does need to be admitted to hospital, the physiotherapy team can assist the paramedics – for example, by sharing information about the person’s specific needs, including use of the correct chair and reasonable adjustments. In hospital, the physiotherapists can discuss the patient’s care with the consultant or other staff and train staff on using specialist kit such as a cough assist machine or oscillating vest. In one case, a physiotherapist supported a person while in A&E who had a tracheotomy and was on a ventilator.
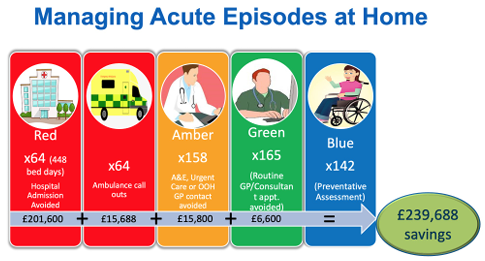
The outcome
From avoiding hospital admissions or reducing length of stay, the team, which now has the equivalent of 6 full time staff, estimates that in 2023 they saved £1 million in cost: a hospital admission due to asthma can cost £1,516 to £2,473 a night and an intensive care bed for a patient with a tracheotomy can exceed £3,000 a night.
Wider impact
The service was extended in November 2023 to include a virtual ward (also known as hospital at home) for anyone whose condition was acquired in childhood. People receive the tests and treatments they need, when they need them but in their home or care home. Just as if they were in hospital, people are reviewed daily and their recovery is monitored by clinical staff.
Members of the team have attended respiratory team meetings and met consultants at the hospital to explain how their service can prevent readmissions.
The team are working to improve their care offer to adults, many of whom are non-verbal. For example, they visit adults even when they are well to help pick up subtle signs of conditions like aspiration pneumonia that carers may not notice. Many of these people are not under the care of a consultant and a GP is unlikely to see the patient often enough to pick up early signs. This shifts the culture from treatment to prevention.
The team has also been trained to have ReSPECT conversations with their patients, and their family or carers, to ensure the person’s wishes are considered should emergency care be required.
They presented their work at a national learning disability physiotherapy conference in autumn 2024 and have shared what they have learned with other NHS trusts.
Their advice for those interested in establishing a similar pathway is:
- invite clinicians, nursing leads or ICS staff to visit patients (with their permission) in their home with you. Seeing first-hand how the service helps people and their families will have more impact than any networking
- ensure you provide self-care training for parents and carers, as the best scenario is that the unwell person remains with someone who knows them and their routine best
- find allies among paediatricians and members of your ICS to support and endorse your work to their colleagues
- create a business case for establishing the service
Contact
The team is happy to be contacted for more information about their service:
Resources
- The Lincs Complex Needs Rapid Respiratory Service: This website includes Chloe’s story, a video showing how the physiotherapy team cared for her
- The Association of Paediatric Chartered Physiotherapists (APCP):
- Evaluation of the 12 month pilot in the Lincs children's service
- A guide to commissioning and evaluation – this includes a new risk identification matrix (2024) for children and young people with neurological impairment. It is hoped that healthcare professionals can use this to improve care, manage co-morbidities and establish new services
- LeDeR resource bank – respiratory resources on aspiration pneumonia, vaccinations, sleep apnoea and more
Improving respiratory health and preventing hospital admissions – Bradford
 Community acquired pneumonia (CAP; from breathing in bacteria or viruses) and aspiration pneumonia (from inhaling food, fluid or saliva) are more common in people with a learning disability than the general population. [*1]
Community acquired pneumonia (CAP; from breathing in bacteria or viruses) and aspiration pneumonia (from inhaling food, fluid or saliva) are more common in people with a learning disability than the general population. [*1]
CAP is a major cause of death and increases the risk of hospital admission in people with a learning disability. Hospital stays can often be long, discharge from hospital complex and people are more likely to be readmitted. [*2]
People from minority ethnic groups can also experience significant barriers in accessing healthcare and much poorer health outcomes. [*3] In Bradford, the average age at death for a person with a learning disability identified as White British was 56 in 2022 but just 26 for someone from an ethnic minority group.
Local LeDeR data found that respiratory disease was associated with 70% of these deaths.
1 British Thoracic Society (March 2023). Statements on community acquired pneumonia and aspiration pneumonia (March 2023)
2 Khurana H, Mckie A, De’vries C, Chhabra H (Nov 2023). Audit of readmissions in patients with learning disabilities. Future Healthcare Journal
3 NHS Race and Health Observatory and University of Central Lancashire (July 2023). We deserve better: Ethnic minorities with a learning disability and access to healthcare
The challenge
The Learning Disabilities team at Bradford District Care NHS Foundation Trust recognised the need to shift from responding when people become unwell to a more preventative, proactive model of care for respiratory health. They also recognised the need for accessible, fully translatable educational resources.
Their considerations were:
- multidisciplinary team (MDT) working – an MDT approach is essential because a range of different health conditions can contribute to the complex risk factors for respiratory health
-
complex medical needs – the trust supports people with complex needs; some depend on interventions such as CPAP, cough assist or suction machines just to remain well
- language barriers – English is not the first language of many of the families the team supports
- raising skills levels – many families/carers provide support with chest physiotherapy, CPAP, cough assist and suction, as well as safe eating and drinking and good mouth care, or employ personal assistants directly or with personal health budgets. Training and resources can help them all
- digital services – a ‘digital hub’ for all respiratory care information would link people with respiratory risk and their carers to the local resources and services they need. Information needs to be accessible, including translations
- financial impact – the team’s conservative estimate (based on data from The King’s Fund 2021) for the cost of a hospital admission due to CAP is £7,000, based on a 7-day stay; many stays are longer. The average cost [*4] of a person attending A&E by ambulance in 2022/23 was £417 and an ambulance call out (with no A&E visit) £287
The response
The team received funding from the trust to create a new multidisciplinary respiratory pathway to reduce chest infections requiring antibiotics and unplanned hospital admissions. They did this with insights from people with lived experience, family members/carers and health colleagues across all disciplines that can have a role in respiratory health.
The pathway is used to identify people with a learning disability who are at the highest risk of respiratory illness, ultimately preventing hospital admissions, improving quality of life, reducing avoidable deaths and reducing costs to the NHS.
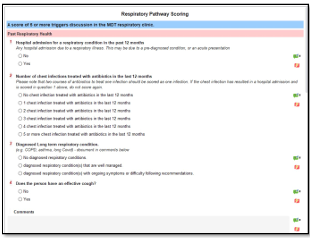 It considers everything that can affect a person’s chest health and increase their risk of respiratory illness and uses a simple scoring system to assess their level of risk. It asks, for example: Does the person’s body shape affect their breathing or digestion? Do they cough when eating or drinking? Do they have epilepsy? Do they have issues with oral hygiene? The scoring system is regularly reviewed and reflects guidance from the National Institute for Health and Care Excellence (NICE) and the British Thoracic Society on aspiration pneumonia and community acquired pneumonia.
It considers everything that can affect a person’s chest health and increase their risk of respiratory illness and uses a simple scoring system to assess their level of risk. It asks, for example: Does the person’s body shape affect their breathing or digestion? Do they cough when eating or drinking? Do they have epilepsy? Do they have issues with oral hygiene? The scoring system is regularly reviewed and reflects guidance from the National Institute for Health and Care Excellence (NICE) and the British Thoracic Society on aspiration pneumonia and community acquired pneumonia.
The team produce a personalised Keeping my Chest Healthy care plan for anyone identified as at risk of respiratory illness. They are piloting a digital version of this care plan.
This plan describes everything the person and their support network can do to reduce this risk, the soft signs of deterioration and the person’s baseline readings to help carers recognise promptly when a person is becoming unwell. It also gives actions people can take if they are becoming unwell and information for staff if the person requires hospital admission. If a person’s health needs change, the team update the plan.
 The team worked with the University of Bradford’s Digital Media Working Academy to develop the Keeping My Chest Healthy digital hub, which works on desktops and smartphones. Care plans have a scannable QR code that links to the digital hub, where users can find fully translatable co-produced information about the risk factors for respiratory disease. Short videos explain the interventions that may be listed in a care plan. For example, if a person’s plan suggests they need support to clear their chest, it will signpost them or their carers to videos showing breathing activities or how to carry out chest physiotherapy. The use of VirtTuri avatars in the videos improves accessibility. These artificial intelligence (AI) avatars can speak over 120 languages, and those used currently can speak in English and Urdu, to reflect the community’s main languages. The videos are also useful for people who are not good readers.
The team worked with the University of Bradford’s Digital Media Working Academy to develop the Keeping My Chest Healthy digital hub, which works on desktops and smartphones. Care plans have a scannable QR code that links to the digital hub, where users can find fully translatable co-produced information about the risk factors for respiratory disease. Short videos explain the interventions that may be listed in a care plan. For example, if a person’s plan suggests they need support to clear their chest, it will signpost them or their carers to videos showing breathing activities or how to carry out chest physiotherapy. The use of VirtTuri avatars in the videos improves accessibility. These artificial intelligence (AI) avatars can speak over 120 languages, and those used currently can speak in English and Urdu, to reflect the community’s main languages. The videos are also useful for people who are not good readers.
The hub supports professionals too, with information on health checks, healthy weight, smoking and the risks around chest health. It also includes guides on taking baseline readings, using a pulse oximeter and recognising sepsis.
From early 2025 the hub will include CPD accredited training modules demonstrating each stage of the pathway, including the scoring and other clinical tools.
Outcomes
By December 2024, over 200 people with a learning disability in Bradford had a Keeping my Chest Healthy care plan. In a random sample of these, over 12 months chest infections treated with antibiotics fell by 54% and hospital admissions for a respiratory condition by 70%.
In the 12 months before one young man had a respiratory care plan, he had 4 chest infections requiring antibiotics and 5 hospital admissions for aspiration pneumonia. At one point his father was advised he was unlikely to recover. In the year after the man had a care plan, he has not had a chest infection or aspiration pneumonia.
Between December 2023 and September 2024, the Keeping My Chest Healthy digital hub had 3,236 unique users, 12,763 page views, 37,674 interactions and 100% positive feedback.
Families and carers who use the hub report feeling 40% more confident that they are providing the right respiratory support. One family member said how much they valued the videos in Urdu as hospital staff had only shown those in their family who spoke English how to use a suction machine.
Wider impact
The team shared this pathway with primary care staff who complete AHCs, asking them to refer anyone they identify at greater risk of developing respiratory disease. They also shared it with acute trusts and are working with other trusts to pilot the pathway.
Any individual who has an acute hospital admission for a respiratory condition is now considered for a Keeping My Chest Healthy plan to improve their chest health and prevent readmission.
In September 2024 this project was recognised as the learning disability initiative of the year at the Health Service Journal patient safety awards.
Contact
For more information please contact:
Resources
 Keeping My Chest Healthy
Keeping My Chest Healthy- RightCare: Learning disability and aspiration pneumonia scenario
- British Thoracic Society: Diagnosis and management of aspiration pneumonia and Diagnosis and management of CAP in people with a learning disability
- NHS England: Continuous positive airway pressure (CPAP) resources
- Royal College of Speech and Language Therapists: Dysphagia guidelines
- NICE: Pneumonia in adults – diagnosis and management
- LeDeR resource bank
Reducing health inequalities – Greater Manchester
The 2023 LeDeR Report found that 39% of reported deaths of people with a learning disability were the result of conditions that can largely be prevented or effectively treated. The percentage of avoidable deaths for the general population was 22% (in 2022).
The top 3 causes of avoidable death for people with a learning disability in 2023 were flu and pneumonia, digestive cancers and ischaemic heart diseases.
Greater Manchester Integrated Care Partnership is working to address health inequalities for people with a learning disability across its 10 localities and almost 3 million population.
The challenge
In 2021/22 only 66% of people with a learning disability in Greater Manchester had an annual health check (AHC). Some did not because they were not on the learning disability register, but some who were did not have the support they needed to engage with services. Isolated and homeless people in particular need additional support.
GP practices may struggle to prioritise AHCs for people with a learning disability because of capacity challenges, particularly if they do not understand the wider benefits.
The response
 The 10 localities in Greater Manchester are tackling the above challenges together through locality ‘Good Health’ groups. These meet regularly and bring together population health colleagues who work with community learning disability teams, local authorities and voluntary, community and social enterprise sector representatives.
The 10 localities in Greater Manchester are tackling the above challenges together through locality ‘Good Health’ groups. These meet regularly and bring together population health colleagues who work with community learning disability teams, local authorities and voluntary, community and social enterprise sector representatives.
By pooling funding the localities have recruited additional primary care assistant practitioners (PCAPs) and learning disability care co-ordinators (LDCCs) to help patients access AHCs, vaccinations and cancer screening. For example:
- Pennine Care NHS Foundation Trust has employed 5 PCAPs in its community learning disability teams; they have a focus on underserved communities and those not engaging with services
- in Bury, the GP Federation pooled Additional Roles Reimbursement Scheme (ARRS) funding to employ 4 LDCCs, one covering each primary care network
There are now over 20 LDCCs across the 10 localities.
Initiatives led by primary care staff, community learning disability teams and the health inequality leads across Greater Manchester to increase AHC uptake include:
- working with local SEND (Special Educational Needs and Disability) designated clinical officers to add a prompt to the Education Health and Care Plan (legal document describing the special educational needs of a child or young person under 25) that the child or young person should be added to the GP learning disability register
- events and educational sessions in specialist high schools/colleges
- training for GPs working in the most deprived localities on offering AHCs
- education sessions at events with ethnic minority groups
- a targeted monthly communication to primary care
Initiatives to increase screening accessibility include:
- Bowel screening: in a pilot in Bury, bowel cancer screening improvement leads worked with the North West Screening Hub, primary care staff, community learning disability teams and PCAPs to support people with a learning disability who were invited for screening or a colonoscopy, and with social care providers to support people in their care to use a FIT kit. They provided easy read information and desensitisation techniques where needed. This pilot was rolled out across Greater Manchester in early 2024 and bowel screening uptake in the learning disability population is now over 75%.
- Targeted lung health check (THLC): people aged between 55 and 74 I who are or were smokers are eligible for a TLHC. Reasonable adjustments are available in this new pathway for people with a learning disability and their invitation to the mobile screening vehicle includes links to easy reads. The health inequalities team is providing bespoke learning disability and autism awareness training to TLHC staff.
- Cancer: the Learning Disability and Autism Cancer Network works to increase screening and accessibility and has representatives from learning disability and cancer services across Greater Manchester. It is developing a reasonably adjusted cervical screening pathway and cancer awareness session for people with a learning disability. The network is also leading the development of a new breast screening charter – every breast screening team in Greater Manchester will pledge to make reasonable adjustments for people with a learning disability: for example, visits to the unit beforehand, longer appointments and having support.
The outcomes
Improved access, experience and outcomes for people with a learning disability are already being seen.
This is illustrated by a 40-year-old man on the GP learning disability register who is homeless and dependent on drugs and alcohol. As he had not been seen in primary care for over 4 years and he was referred to the community learning disability team and assigned a PCAP. The PCAP worked with the primary care team and the nurse from Turning Point (a drug and alcohol service) to engage him, assess his health and provide ongoing support. The PCAP even met him after an appointment at the Court of Protection where he was encouraged to stay for his first flu vaccination.
Another person who struggled with drug and alcohol use and literacy difficulties was referred to the PCAP service having declined 3 invitations for an AHC. The PCAP’s visits were invaluable in understanding the person’s needs and the support and reasonable adjustments they needed, as well as in building rapport. This person has since attended AHCs and other appointments.
AHC uptake in Greater Manchester increased from 66% in 2021/22 to 81.3% in 2023/24. Stockport East & South PCN had a 99% completion rate and the Bury locality achieved a 34.1% increase over the 2 years.
The health inequalities lead for Greater Manchester suggests that anyone wanting to recruit more support roles to tackle health inequalities works with their ICB’s personalised care team to raise awareness of the impact these roles can have, as well as the ARRS funding available.
Contact
For more information on any of the initiatives, please contact:
Resources
- NHS e-learning for health: Caring for people with a learning disability - Health inequalities and social deprivation for medical professionals - Greater Manchester learning disability strategy
- The Greater Manchester Cancer Podcast: - This podcast presented by Steve Bland of the BBC podcast ‘You, Me and the Big C’, includes an episode exploring health inequalities in the cancer system
- LeDeR resource bank –respiratory resources on tackling health inequalities and more
Managing medication and constipation risk – Surrey
In 2023, a University of Central Lancashire and King’s College London report identified that almost half of a sample of96 people who had a LeDeR review in 2021 had constipation, and over half of had been prescribed medications that can cause constipation – on average at least 2: opiates, antipsychotics, antidepressants, antiepileptics, antispasmodics and antimuscarinics.
While constipation was not given as a cause of death on any of the death certificates, 30% of those with constipation did have conditions on their death certificate that are associated with or caused by constipation (for example, bowel cancer, sigmoid volvulus, sigmoid perforation, bowel obstruction).
Few people in the sample had been taught about what normal bowel habits are, yet laxative prescriptions for constipation were also very common. Laxatives should never substitute for a healthy diet, adequate hydration and exercise.
Medication reviews should be delivered as part of a person’s annual health check (AHC) to ensure they are receiving the right medication for their needs, and every AHC should be supported with a health action plan for the individual.
The challenge
 Local LeDeR reviews in Surrey Heartlands ICS identified concerns about medication reviews, specifically in relation to the management of polypharmacy and constipation. One review for a person with a history of constipation identified a lack of care planning, monitoring of bowel habits and escalation of concerns following a medication review.
Local LeDeR reviews in Surrey Heartlands ICS identified concerns about medication reviews, specifically in relation to the management of polypharmacy and constipation. One review for a person with a history of constipation identified a lack of care planning, monitoring of bowel habits and escalation of concerns following a medication review.
The quality of completed AHCs and medication reviews is not measured.
The response
The local LeDeR co-ordinator asked the Surrey and Borders Partnership Trust pharmacy team to audit prescribing and completed medication reviews and AHCs for people with a learning disability on polypharmacy and who had, or were at risk of, constipation.
With the regional LeDeR co-ordinator and Surrey Heartland’s Medicines Safety Officer, the project team worked with GP practices to identify people who:
- had a learning disability aged 14 and over and on the GP register
- had a diagnosis of constipation recorded on EMIS
- were prescribed medicines for constipation (laxatives)
- were at risk of constipation from prescribed medications medications (opiates, anti-psychotics, anti-depressants, anti-epileptics, antimuscarinics and antispasmodics)
- were prescribed 10 or more medicines (polypharmacy)
 They did this by running EMIS searches, the system holding electronic patient records. In the 7 participating GP practices (serving a registered population of about 70,000), this identified 359 patients who met one or more of the following criteria:
They did this by running EMIS searches, the system holding electronic patient records. In the 7 participating GP practices (serving a registered population of about 70,000), this identified 359 patients who met one or more of the following criteria:
- 316 had received an AHC in the last 18 months (86.8%)
- 26 had a constipation diagnosis recorded on EMIS (12.6%)
- 128 were prescribed medicines for constipation (laxatives; 34.5%)
- 220 were at risk of constipation from prescribed medicines (61.6%)
- 100 were prescribed 10 or more medicines (polypharmacy; 25.3%)
A detailed ‘thematic’ review of 156 randomly selected records identified good practices around AHCs and medication reviews in some GP practices, such as:
- a nurse performing an AHC followed by the practice pharmacist conducting a medication review
- personalised AHC content, not a ‘tick box’ approach
- good quality and individualised constipation care plans
but also inconsistencies in others such as:
- unclear or inconsistent documentation of both care planning and AHC outcomes
- for people with a history of constipation, high-risk prescribing not always addressed
- variability in the involvement of a carer or family member
- variability in how AHCs were documented and the templates used
- inadequate collaboration across care settings, for example shared records
- discrepancies between number of constipation diagnoses recorded and number of people treated for constipation
The outcome
The evaluation demonstrated that completion rate is too crude an AHC performance measure as it gives no indication of the quality of AHCs and medication reviews.
- The pharmacy team recommended the following actions to improve health outcomes:
- constipation care planning with high-risk populations, for example people with a history of chronic constipation, complications, antipsychotic polypharmacy
- review medicines that cause constipation
- implement the STOMP and STAMP principles (to stop inappropriate prescribing of psychotropic medications)
- a standardised template for AHCs
- greater collaboration across care settings, for example sharing records
- improved documentation of, for example, AHCs and constipation diagnoses
While the audit was not intended to be interventional, the pharmacy team did escalate their clinical concerns regarding 2 at-risk patients.
The team shared their findings and recommendations with the GP practices that took part, the Learning Disability Quality Assurance Group and non-medical prescribers’ group at Surrey and Borders Partnership Trust, as well as widely across the system, including with the Surrey Heartlands Learning Disability Integrated Partnership Board and Patient Safety Group. They ran a ‘lunch and learn’ session for primary care staff (GPs, pharmacists and advanced specialist nurses) across Surrey Heartlands.
The team is working with local commissioners to embed their recommendations concerning polypharmacy and constipation. They are also making a system-wide case for a specialist pharmacist for learning disability role in the trust who can advise primary care staff on reviewing their prescribing for people with a learning disability. This could help those GPs who are hesitant to do so because they consider this a specialist area.
The team have also used NHS England funding to design and deliver a training package for primary care on conducting structured medication reviews. In July 2024, 40 clinicians working in PCNs attended the course and learned how to identify the red flags for patients at risk of constipation, engage specialist help when needed and deprescribe inappropriately prescribed psychotropics, and how primary care learning disability liaison nurses can also help with this process.
For other areas wanting to conduct a review of medication, AHCs and management of constipation, the team suggests:
 involve people with lived experience in service design and evaluation
involve people with lived experience in service design and evaluation- ask key people across your network for help from the outset, starting with the ICB medicines management team
- emphasise to busy GPs the value of an audit and training to improve the lives of those with a learning disability
- primary care clinicians ask ‘why?’ when someone does not attend their AHC
Contact
For more information please contact:
 Resources
Resources
- NHS England: Constipation resources for people with a learning disability
- NHS England: Constipation campaign toolkit
- LeDeR resource bank – constipation guidance and resources
- NHS England: STOMP and STAMP website
- NHS England: Poo Matters – resources for healthcare professionals
Ensuring cardiopulmonary resuscitation (CPR) decisions for people with a learning disability are made well – South West
The challenge
The NHS is clear that ‘learning disability’ and ‘Down’s syndrome’ should never be recorded as a reason for do not attempt cardiopulmonary resuscitation (DNACPR) decisions, or used to describe a person’s immediate or direct cause of death.
LeDeR reviews continue to highlight issues for people with a learning disability and their families around informed choices for end of life care and decisions around CPR.
The response
In 2023 the South West region audited patient notes for people with a learning disability to understand how treatment was escalated and CPR decisions made for this group. Each of the region’s 7 ICSs reviewed the records of up to 100 living patients with a learning disability in their area. The NHS England South West LeDeR Operational Group acted as the steering group for this audit.
Specifically, the audit considered if appropriate steps are being taken to discuss treatment options with a person and document their wishes in a treatment escalation plan should their health deteriorate, and how CPR decisions documented in hospital records had been made for people with a learning disability. The plan should reflect a person’s values and decisions on treatments, for example ventilation, blood transfusion as well as CPR. All staff treating the person should refer to it and it is reviewed whenever a patient is readmitted to hospital.
ICSs assessed CPR decisions by collating data from patient records. This information was then further considered within structured interviews with key staff.
 Auditing hospital records: As some ICSs in the South West use the ReSPECT (Recommended Summary Plan for Emergency Care and Treatment) form developed by the Resuscitation Council UK and others use a local treatment evaluation plan, 2 versions of the audit form were needed. Both forms used a combination of ‘yes/no’ and free text responses.
Auditing hospital records: As some ICSs in the South West use the ReSPECT (Recommended Summary Plan for Emergency Care and Treatment) form developed by the Resuscitation Council UK and others use a local treatment evaluation plan, 2 versions of the audit form were needed. Both forms used a combination of ‘yes/no’ and free text responses.
ICSs were expected to answer a set of core questions agreed by the steering group, but they could add locally applicable questions if they wished. The questions asked:
- whether learning disability was recorded as the sole reason for DNACPR (something that should never happen)
- how the person’s mental capacity had been assessed and documented
- whether the person, their family or advocate were involved in discussions about resuscitation status
- whether the person had an advanced care plan documenting their individual preferences and priorities for care and if this was followed
One ICS used the local audit team to complete the audit forms while the others used ICS staff or staff from acute hospital teams, such as junior medical staff or lead nurses. 6 ICSs referred to patient data in the acute care record, with some including outpatient data; 1 ICS collated data from primary care records.
Interviews: A commissioning support unit conducted semi-structured interviews with 10 core members of acute and community-based teams to probe issues identified by the audit results: advanced care planning; how and when conversations about a person’s wishes might take place; and applying the Mental Capacity Act in CPR planning for people with a learning disability. Those interviewed included a community learning disability nurse, a GP, a palliative care nurse, a safeguarding adults and Mental Capacity Act lead nurse, a palliative care consultant and a chief nursing officer.
The outcome
The South West ICSs audited 589 patient records and found:
- 11% of records with a DNACPR in place for the person gave ‘learning disability’ as a reason for DNACPR alongside other health condition(s); it was recorded as the sole reason in only 1 record
- the Mental Capacity Act was not always applied properly; that is, reasonable adjustments were not always made to assist a person’s decision-making and capacity assessments were not always clearly documented
- 20% of people were involved in discussions about their CPR status
- family or next of kin were involved in 63% of discussions about CPR status
- learning disability acute liaison nurses often acted as the catalyst for communication with family members around CPR decision-making and application of reasonable adjustments in acute settings, in some cases advising that capacity decisions should be changed and helping to ensure that ‘best interest’ processes were followed
These findings suggested the following actions for the region:
- share a single advanced care plan across local health and care systems
- focus on increasing the completion of advanced care plans by people when they are well and with the support of the people who know them best
- trusts’ Mental Capacity Act training should include how to apply reasonable adjustments for people with a learning disability and autistic people
- use of ‘learning disability’ as a sole reason for DNACPR on CPR forms should be explicitly identified as inappropriate, supported by clinical leaders and training
- engage people who know the person well in CPR decisions, particularly where the person has a profound and multiple learning disability
EacEach ICS is creating an action plan for system-level improvements based on learning from its own local audit. ICSs will then re-audit to evaluate the impact of their improvement programme, but some changes are already showing an impact:
- Bristol, North Somerset and South Gloucestershire: the CPR plan now states at the top that ‘learning disability’ is not a reason for DNACPR, the Chief Medical Officer has told staff that it is not acceptable and staff training around this has been provided.
- Devon: has increased community access to forms by rolling out an electronic version of the ReSPECT form, and improved form completion by increasing staff training
- Gloucestershire: working with the Resuscitation Council UK and Inclusion Gloucestershire, has produced 2 videos for people with a learning disability about the ReSPECT process: Jenny and John’s stories. It has also co-produced easy read guides and presented to learning disability providers about ReSPECT
- Cornwall: has developed an easy read leaflet about completing treatment escalation plans. Also, Cornwall People First is running ‘speak up’ groups with a counsellor where people with a learning disability can discuss their experiences of death, dying and loss
- Somerset: is piloting an advanced care planning clinic for people with a learning disability and their family/carers. It is also trialling a part-time post in the end of life care education team to train and support staff working with people with a learning disability. The LeDeR team commissioned the video We need to talk about death
Contact:
For more information about this audit, please contact:
Resources
- NHS England: resources to ensure equality in palliative care
- NHS England: Universal principles for advance care planning (an easy read version is available)
- East and North Hertfordshire NHS Trust: Treatment escalation planning – information for patients
- LeDeR resource bank – end of life care resources and guidance
Helping people who live in a care home to manage their weight – Norfolk
 People with a learning disability are more likely to be obese than the general population [5], with poorly balanced diets and low levels of physical activity. Excess weight can cause illness, disability and premature mortality. There are also close links to social disadvantages such as poverty or social isolation, which people with a learning disability disproportionately experience. [6]
People with a learning disability are more likely to be obese than the general population [5], with poorly balanced diets and low levels of physical activity. Excess weight can cause illness, disability and premature mortality. There are also close links to social disadvantages such as poverty or social isolation, which people with a learning disability disproportionately experience. [6]
The 2023 LeDeR report identified ischaemic heart disease is the 3rd most common avoidable cause of death for people with a learning disability (9.5%); this can be caused or worsened by excess body weight. Carrying extra fat can also lead to stroke and Type 2 diabetes, and is linked to some cancers, for example breast and colon.
The challenge
The specialist learning disability dietitians in Norfolk Community Health and Care NHS Trust wanted to ensure that people with a learning disability, their families and carers were receiving good dietary advice around healthy eating and weight loss, and that this was accessible to them.
They also considered that staff in care homes or supported living settings, who have a duty of care to support people to eat well, needed clearer information as adults with a learning disability who live in residential homes do not necessarily make their own food choices. [7]
The response
Norfolk and Waveney ICS established a LeDeR nutrition group in 2023, bringing together specialist learning disability dietitians and staff from other disciplines.
The group ran a 6-month weight management pilot with a 20-bed private residential home for people with a learning disability near King’s Lynn. Residents live independently and staff provide support with meals.
The dietitians supported staff in managing the diet of 8 overweight residents who were on a weight management plan. At the end of the pilot they sent each of these resident’s GP a discharge letter summarising any interventions and advising the GP to re-refer in 3 months if the person did not lose weight.
 They also provided care home staff with:
They also provided care home staff with:
- their ‘Weight Management Pack for Carers’, which has chapters on healthy eating, portion size, food labelling, healthy snacks, drinks and fluids, takeaways, meal planning, changing eating habits, salt and the importance of physical activity
- an informal session with a learning disability nurse to explain how the pack could be used with residents to encourage healthier eating, meal planning and higher levels of physical activity
- advice on engaging other support services and details of how to do so if they needed more support with any resident’s weight management or eating; for example, community learning disability teams, speech and language therapists, physiotherapists or psychologists for residents with dysphagia, posture issues or behaviours relating to food
- a ‘Statement of Responsibility’ for each person on a plan to promote healthier eating
 a reminder that it was their statutory duty of care to the person[8] to look after their nutritional and hydration needs and that, where residents lacked the mental capacity to make informed choices on healthy eating, they needed to follow ‘best interests’ processes
a reminder that it was their statutory duty of care to the person[8] to look after their nutritional and hydration needs and that, where residents lacked the mental capacity to make informed choices on healthy eating, they needed to follow ‘best interests’ processes- the suggestion that they spent an hour a week with each resident going through the weight management pack to review the changes required in eating habits and activity levels
Social prescribing link workers visited the home to suggest activities.
The outcomes
The pilot highlighted that individuals need time and support to change their eating habits and that, where staff are concerned about residents’ eating and relationship with food, they should link with learning disability nurses to create support plans with residents.
After 6 months – the end of the pilot – 4 individuals had lost weight and 4 had gained weight. The care home staff felt that:
- the pilot would have had more success over 12 months as that is how long it can take people to make changes around food
- taking 1 hour a week to review each resident’s progress using the pack is resource intensive, but staff do use the pack with individuals when time allows
- residents are more likely to listen to messages that do not come across as “nagging”, and dietitians/social prescribers could potentially support staff to deliver messages more positively
- having more involvement from dietitians and social prescribers could keep staff more focused on supporting and safeguarding residents in relation to weight management
The care home has continued to make the advised changes gradually and is now seeing more positive results, with more residents having lost weight and becoming fitter, and the home’s food choices and portion sizes are improving. For example, staff now help residents who have a kitchen to plan and prepare meals or cook for other residents. Although this has not always been easy, staff have persevered with the use of lower fat meats, fewer processed foods, lighter mayo and less sauce on food. Some residents have cut down on how much meat they eat and all are eating more vegetables.
One overweight resident who initially did not want to go on a ‘diet’ or to eat ‘healthy food’ has now lost weight because care home staff took the time to use the pack and explain that what she would be doing is making healthier choices in the meals she ate and portion sizes.
Another resident was reluctant to cut down on eating half a packet of biscuits and 3 packets of crisps a day. Staff encouraged her to replace this with 2 ‘snack pots’ each containing half a packet of crisps, dried fruit and a cereal bar. The staff explained that ‘diet’ food or drinks should still be regulated and, while healthier, fruit should be eaten in portions. The resident has also swapped toast for porridge/muesli and has lost some weight.
Residents now regularly attend a small local gym, 1 goes on a fitness bike every day and others cycle around the grounds on a tricycle.
A resident who weighs nearly 30 stone (190 kg) was struggling to stand and had lost muscle mass. He was not among those who lost weight during the pilot, likely because he chooses his own food and meals when he leaves the home. However, since the pilot, he has started regularly attending the gym and finds it much easier to stand.
Feedback on the pilot from staff and residents helped the dietitians update the pack and, working with the Opening Doors self-advocacy service, develop an easy read version for use in care homes, supported living settings and by families and carers. It has also informed the delivery of training in using the weight management pack, which reiterates monitoring a person’s weight at annual health checks.
Advice for carers supporting people to lose weight includes:
- run sessions in rooms with no other distractions
- understand levels of mental capacity: for example, a care home resident may have ‘functional’ capacity to decide to eat healthily but lack ‘executive’ capacity to act on this, so carers need to act on their behalf in their best interests
- physical activity is not something that needs to be done in a formal exercise class
- avoid using food as a reward
Contact
For information or a copy of the weight management pack (which is not online), please contact the learning disability dietitians:
Resources
 NHS Managing Your Weight
NHS Managing Your Weight - NICE guidance: Obesity prevention
- OHID: Obesity and weight management for people with learning disabilities
- LeDeR resource bank: resources on diabetes / weight and constipation
- [5] Emerson E (2005). Underweight, obesity and exercise among adults with intellectual disabilities in supported accommodation in northern England. Journal of Intellectual Disability Research
- [6] Public Health England. Obesity, weight management and people with learning disabilities
- [7] Hoey E, et al (2017). An examination of the nutritional intake and anthropometric status of individuals with intellectual disabilities. Journal of Intellectual Disabilities
- [8] See: Regulation 14 of the Health & Social Care Act 2008: Meeting Nutritional and Hydration Needs
National initiatives that can be used locally to improve services for people with a learning disability and autistic people
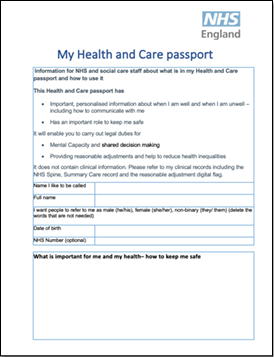
Health and care passports
 A health and care passport (also known as a hospital passport) summarises information about a person’s healthcare needs, how they communicate, key ‘do’s’ and ‘don’ts’ to inform care planning, key people in their network and reasonable adjustments that can support safe and effective care quickly. This content is owned by the person – what they want health and care staff to know about them for delivery of effective care. It does not replace clinical records and should not be used to record clinical decisions.
A health and care passport (also known as a hospital passport) summarises information about a person’s healthcare needs, how they communicate, key ‘do’s’ and ‘don’ts’ to inform care planning, key people in their network and reasonable adjustments that can support safe and effective care quickly. This content is owned by the person – what they want health and care staff to know about them for delivery of effective care. It does not replace clinical records and should not be used to record clinical decisions.
The passport, which can be a paper or digital document or both, should be portable across health and care services, accessible to staff as needed and updated should the person’s health needs change, to support delivery of personalised care by clinical or administrative staff.
The challenge
Health and care passports are used variably across the country and there is inconsistency in the information they collate. Some ICSs have invested significant resources and worked closely with people with lived experience to produce a passport for use across their area; others are just beginning this work.
The Health Services Safety Investigations Body’s (HSSIB) report in November 2023, Caring for Adults with a learning disability in acute hospitals, recommended that NHS England “…develop and publish a set of guidelines on information to be included in a health and care passport… for people with a learning disability with consideration of the reasonable adjustments that people may need”.
The response
NHS England worked with representatives from ICSs, NHS trusts and people with lived experience to develop resources for ICSs and partners in the voluntary and independent sectors. It published implementation guidance for health and care passports and a template passport in June 2024.
The national template is intentionally a ‘health and care passport’, not a ‘hospital passport’ – as hospitals play only a small part in a person’s health and care, and the information in the document is relevant across health and care, including primary and community care.
What health and care organisations need to do
When people with a learning disability attend NHS appointments, staff should ask for the person’s health and care passport and use the information it contains to inform their approach to supporting, assessing and treating them. They should provide any reasonable adjustments that are needed.
If someone does not have a passport or it is not up to date, staff in the NHS and in care organisations should encourage and support people with a learning disability to develop one or make sure that the information in their passport is up to date and complete.
ICSs should follow the guidance, review their arrangements for the implementation of the health and care passport, check their local template is consistent with the national template in terms of the information it collates, and ensure staff are aware of the value of these passports for safe, effective and personalised care.
The Reasonable Adjustment Digital Flag is being implemented across the NHS and publicly-funded social care to support individuals who require health and care services to make reasonable adjustments for them, as described below.
The flag can be used to indicate that a person has a health and care passport and how to access it.
 Resources
Resources
- NHS England: Health and care passports: Implementation guidance
- NHS England: Health and care passport template
- Download the template and plain English guide
- NHS England: Health and care passport: Easy read Information about what a health and care passport is and how to complete one
- Reasonable adjustments – case studies of reasonable adjustments in action
Implementing the Reasonable Adjustments Digital Flag (RADF)
 Under the Equality Act 2010 all organisations have a legal duty to ensure that their services are as accessible to people with a disability as they are to anyone else – by making ‘reasonable adjustments’ where a person needs these, whenever and wherever they are seen and treated.
Under the Equality Act 2010 all organisations have a legal duty to ensure that their services are as accessible to people with a disability as they are to anyone else – by making ‘reasonable adjustments’ where a person needs these, whenever and wherever they are seen and treated.
Access to services is often equal, but not equitable or fair. The RADF supports organisations to meet their legal obligations under the Equality Act, ensuring that people with a disability have reasonable adjustments where they need these to access care, and positive experiences of and outcomes from services.
The challenge
The reasonable adjustments a person requires need to be identified, recorded and shared across the NHS and publicly-funded care.
While this has been required by law since 2010, until now sharing this information before it impacts on care and service delivery has been difficult. The RADF was created to address this need.
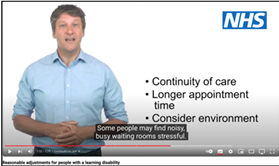
Reasonable adjustments for someone with a learning disability or an autistic person can include providing a longer appointment, demonstrating what’s involved in cancer screening ahead of screening, providing a quiet room, sharing easy read information or involving carer’s support. They are individual to the person.
The response
NHS England has piloted and built a digital flag in the central national repository (which supports health and care IT systems). It is being adopted by health and publicly funded care services across England.
This flag identifies in a patient’s record that they have “a physical or mental impairment that has a substantial and long-term adverse effect on their ability to do normal daily activities” and therefore that they may need reasonable adjustments to remove any access barriers they face because of disability.
The flag should be created by whichever health or care professional knows the person best and has identified the need for a flag. It must give details of the person’s significant impairment(s) and the reasonable adjustments they may need.
All staff with the appropriate security permissions can use the National Care Records Service to record and view flags, and add or remove information from a flag. Over time organisations will also be able to integrate directly with the national asset, allowing users to enter and see the flag's information in their normal electronic patient record.
What health and care organisations need to do
 NHS England published an Information Standards Notice for the RADF, under section 250 of the Health and Social Care Act 2012. This includes a step-by-step guide to implementing the flag in all NHS and publicly-funded social care organisations in England and how to use it, and the RADF action checklist identifies the actions they are required to have completed for full compliance by 31 December 2025.
NHS England published an Information Standards Notice for the RADF, under section 250 of the Health and Social Care Act 2012. This includes a step-by-step guide to implementing the flag in all NHS and publicly-funded social care organisations in England and how to use it, and the RADF action checklist identifies the actions they are required to have completed for full compliance by 31 December 2025.
Health and care staff should find out if people accessing their service have a digital flag and, where needed, put reasonable adjustments in place in advance of their attendance. If someone has a disability and needs reasonable adjustments, but does not yet have a digital flag, health and care staff should talk to the person and their carer, if they have one, and create a flag to ensure their reasonable adjustment needs are met at future appointments.
Full implementation of the RADF is supported by staff training.
Contact:
Please direct all enquiries about flag implementation to the project mailbox:
Resources
- The Reasonable Adjustment Digital Flag action checklist: explains what you need to do to achieve compliance (for health and care providers)
- NHS England: Reasonable Adjustment Digital Flag explained: explains how to support people with a learning disability attending an appointment or annual health check
Glossary
Annual health check (AHC) – this is offered to anyone over 14 who has a learning disability and is on their GP learning disability register. They are important for maintaining a person’s physical and mental health and wellbeing.
Autism –the diagnostic criteria for autism include: differences in social communication and interaction; highly focused interests or behaviours that appear to others as repetitive or restricted; and challenges with sensory hyper or hypo-sensitivity.
DNACPR – do not attempt cardiopulmonary resuscitation (or a ‘DNR’ or a ‘DNAR’) is an advance decision not to attempt cardiopulmonary resuscitation should a person experience cardiac or respiratory arrest.
Diagnostic overshadowing – where a person’s symptoms of physical ill health are mistakenly attributed to a mental health/behavioural problem or as being inherent (that is, exist because of) the person’s learning disability.
Education and health care plan (EHCP) – sets out the education, healthcare and social care needs of a child or young person.
Health action plan – as part of a patient’s annual health check (AHC), GP practices are required to produce a health action plan. This identifies the patient’s health needs, what needs to happen and who will lead on this (including what the patient needs to do) and when the plan will be reviewed. The plan includes any key action points agreed during the AHC.
Integrated care board (ICB) – NHS organisations responsible for planning health services for their local population. There is one ICB in each integrated care system area. They manage the NHS budget and work with local providers of NHS services, such as hospitals and GP practices, to agree a joint five-year plan which says how the NHS will contribute to the ICP’s integrated care strategy.
Integrated care partnership (ICP) – a statutory committee with representation from local government, the voluntary, community and enterprise sector, NHS organisations and others that develop a health and care strategy for an area.
Integrated care system (ICS) – a group consisting of the NHS, councils, voluntary sector and others that work together to improve the health of people in their area. There are 42 ICSs in England.
Learning disability – a disability affects the way a person understands information and how they communicate and is present from childhood. People with a learning disability can find it difficult to understand new or complex information, learning new skills and coping independently.
LeDeR – Learning from lives and deaths – People with a learning disability and autistic people : LeDeR reviews are carried out by ICSs to provide insights to improve care, reduce health inequalities and prevent premature and avoidable mortality of people with a learning disability and autistic people.
LeDeR review – looks at the health and social care that a person with a learning disability or autistic person received before their death. This may have relevance to their overall health outcomes. Reviews are not investigations or part of a complaints process.
NHS Spine – this supports the information technology systems for health and social care in England, linking more than 23,000 systems in 20,500 organisations.
ReSPECT (Recommended Summary Plan for Emergency Care and Treatment) – this is both a process and a form to capture personalised recommendations for someone's clinical care in emergency situations.
SEND (special educational needs and disability) – a child or young person has special educational needs and disabilities if they have a learning difficulty and/or a disability that means they need special health and education support.
Social prescribing – this is when healthcare professionals refer patients to support in the community, to improve their health and wellbeing.
Voluntary, community and social enterprise (VCSE) sector – an integral part of integrated care boards, systems and partnerships that is crucial to supporting the NGS and its partners to deliver the change needed for people with a learning disability.
Acknowledgements
This LeDeR action from learning report gives examples of the vital work that has been delivered across the NHS and by our partners, working with self-advocates and self-advocacy groups, parents/carers, the charity and voluntary sectors, and our colleagues in social care. None of these efforts would be possible without family members, health and social care staff and many others contributing to a LeDeR review by sharing their experience of the life and death of a loved one or someone in their care. We would like to express our sincere gratitude to you all.
We would like to recognise and thank everyone whose work, campaigning or self-advocacy continues to inform, challenge, change and reduce health inequalities among people with a learning disability and autistic people.
We highly value our Independent Advisory Group whose members include people with a learning disability, autistic people, parents and carers, and representatives from the charity and voluntary sectors. They inform and enrich our work. Please see Appendix 1 for its membership.
We are also supported by our academic partnership, comprising King’s College London, University of Central Lancashire, Kingston and St George’s, University of London, which produced the LeDeR Annual Report 2023 as well as the Staying Alive and Well Group who support their work and produced this year’s easy read and video versions of the LeDeR annual report.
Finally, we are grateful to the LeDeR workforce and partners in ICSs across England for their continued efforts to address local LeDeR findings and to improve the health and lives of people with a learning disability and autistic people.
Appendix 1: LeDeR Independent Advisory Group Members
|
Association of Directors of Adult Social Services (ADASS) |
London School of Hygiene and Tropical Medicine (LSHTM) |
|
Department of Health and Social Care (DHSC) |
Office for Health Improvement and Disparities (OHID) |
|
Royal College of General Practitioners (RCGP) |
|
|
Institute of Health Equity – University College London |
|
|
Voluntary Organisations Disability Group (VODG) |
|
|
Local Government Association (LGA) |
|